Canal Knowledge
Posted: August 15, 2011
Last Modified: March 22, 2021
This post addresses a very common situation and question that we encounter in daily practice: the root canal. What is it? And what is involved?
First off, we should talk about a normal tooth. When forming, teeth form from the outside in (roughly), and at the end of the formation phase, a space at the centre of the tooth remains. This is known as the pulp, where live tissue such as blood vessels and nerve tissue reside.
The pulp extends down the roots of the tooth (for a cutaway tooth, see here) until it connects to the larger branches of nerve or blood vessel outside the tooth. This thinner area down the centre of the roots is known as the root canal. The nerves inside the tooth allow it to feel pain (such as when you have something cold to drink), but all this live material is actually useless to the functioning of the tooth once the tooth is formed. The sensation that you get from teeth (such as that which tells you when you have hair in your food) actually arises from nerve fibres outside your tooth, in the periodontal ligament space. So, even if the nerve fibres and assorted other living tissue within the tooth were gone, the tooth would function just fine.
Which brings us to the scenario that we are faced with: what if the living tissue inside the tooth were not healthy? What if it needed to go?
There are several reasons why the pulp of a tooth (along with the tissue in the root canals) might not be healthy, and it usually has to do with compromising of the blood supply to the inside of the tooth.
A pulp can be damaged by simple trauma, cavities that extend to the pulp, or insults such as large fillings or other dental procedures. In any event, if a pulp is damaged beyond repair, it will die. This can occur painfully or not, but the end result is that there is dead material inside the tooth.
Dead material will eventually become infected, and since antibiotics will not reach the inside of a dead tooth (no blood vessels to deliver the antibiotic), the material needs to be physically removed. Root canal treatment to the rescue!
Root canal therapy (or colloquially, root canals, or for the purposes of this post, RCT’s) is a technique that in general involves entering the pulp space of the tooth and physically cleaning out the inside of the tooth of all the dead / dying material. It can also involve other less common pulp treatments, but those are beyond the scope of this article.
The technical procedure of the root canal is often focused on, but really, the important part is the biological objective – what are we trying to do? And disinfection of the inside of the tooth is the ultimate goal, so that the tissues around the tooth are not subjected to a neverending outflow of bacteria and bacterial products. We have files and disinfectant rinses that we use to clean out the pulp spaces of teeth, and regardless of how it’s done, a successful RCT restores the tooth to a clean state.
Once the root canals are disinfected, the cleaned-out area is filled with a dedicated root canal filling material (lots of choices here), and must be finished with a filling to close the access hole created at the beginning of treatment. If enough original tooth material is gone, the frequent recommendation of a crown or onlay is recommended. As good as a root canal may be, the tooth is always left in a weaker condition that an untouched tooth. Crowns/onlays help reduce the risks of further tooth fracture.
From the patient’s perspective, RCT can be compared to a really boring filling appointment. Sure, there are lots of different tools, but not a lot of noise or motion inside the mouth. Bring a music player to pass the time.
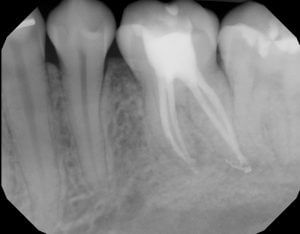
Because people love pictures, here are some x-ray images of a completed root canal in our office. This root canal was deliberately done over two appointments, separated by two months. The first appointment involved all the cleaning and disinfection steps, culminating in the placement of an antibacterial dressing inside the canals.
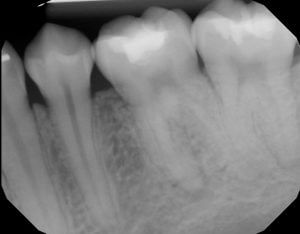

After two months of calcium hydroxide dressing inside the canals, and ensuring that the patient is no longer feeling anything from the tooth, we were confident that the root canal was going to be successful. We proceeded to fill the canals and ultimately fill the top of the tooth with a conventional filling material.
From the outside, one cannot tell if a tooth has had RCT, and if successful, the tooth feels just like any other. Hopefully with proper post-RCT management, the tooth will continue to function anonymously along with all the other teeth!
Hope this clears things up. Thanks for reading, and as always, please contact us for questions regarding your own dental questions and conditions!


